RGUHS Nat. J. Pub. Heal. Sci Vol No: 12 Issue No: 2 pISSN: 2249-2194
Dear Authors,
We invite you to watch this comprehensive video guide on the process of submitting your article online. This video will provide you with step-by-step instructions to ensure a smooth and successful submission.
Thank you for your attention and cooperation.
1Dr. Mallikarjun Kokatanur, Department of Shalya Tantra, Shree Jagadguru Gavisiddeshwara Ayurvedic Medical College and Hospital, Koppal, Karnataka, India
2Department of Shalya Tantra, Shree Jagadguru Gavisiddeshwara Ayurvedic Medical College and Hospital, Koppal, Karnataka, India
3Department of Shalya Tantra, Shree Jagadguru Gavisiddeshwara Ayurvedic Medical College and Hospital, Koppal, karnataka, India
4Department of Shalya Tantra, Shree Jagadguru Gavisiddeshwara Ayurvedic Medical College and Hospital, Koppal, Karnataka, India
5Department of Shalya Tantra, Shree Jagadguru Gavisiddeshwara Ayurvedic Medical College and Hospital, Koppal, Karnataka, India
*Corresponding Author:
Dr. Mallikarjun Kokatanur, Department of Shalya Tantra, Shree Jagadguru Gavisiddeshwara Ayurvedic Medical College and Hospital, Koppal, Karnataka, India, Email: mallikarjunkokatanur@gmail.com
Abstract
Background: Arshas is one of the most common anorectal conditions. In Ayurveda, the term ‘Arsha’ refers to any anorectal projection, including haemorrhoids, skin tags, rectal polyps, and similar lesions. In the present context, Arsha specifically refers to internal haemorrhoids. Both Acharya Charaka and Acharya Sushruta have described four modalities of treatment for Arshas. While Acharya Sushruta emphasizes Kshara, Agni, and Shastra Karma, Acharya Charaka places greater importance on Bheshaja, as it is the most practical method of management with minimal disruption to the patient's daily life. While discussing Alepa Yogas in the treatment of Arsha, Acharya Sushruta described the local application of Kasisadi Taila, where as Acharya Charaka, while explaining Urustamba Chikitsa, has referred to the use of Saindavadhya Taila in Arshas. Therefore, in this study, an effort was made to evaluate the therapeutic effect of Saindavadya Taila administered as Guda Purana, in comparison with Kasisadi Taila.
Methods: An open-label, randomized controlled clinical study was conducted. A total of 40 clinically diagnosed patients of Abhyantara Arshas were selected from the IPD and OPD of SJGAMC and H and randomly assigned to two groups, Group A and Group B, with 20 patients in each group.
Results: The study results indicated that the control group showed a comparatively better outcome than the trial group (P value < 0.05).
Conclusion: The study concluded that both the trial and control groups showed significant improvement in reducing bleeding and constipation. However, the control group demonstrated greater effectiveness than the trial group in reducing the size of the haemorrhoidal mass.
Keywords
Downloads
-
1FullTextPDF
Article
Introduction
Haemorrhoids are the dilated veins within the anal canal in the sub-epithelial region, formed by radicles of the superior, middle, and inferior rectal veins. Internal haemorrhoids are those within the anal canal and internal to anal orifice.1
The incidence of haemorrhoids increases with age, with at least 50% of individuals over 50 years experiencing some degree of haemorrhoidal symptoms.2 The global prevalence of haemorrhoids is estimated to be approximately 4.4%, affecting about 10 million people. Although haemorrhoids can occur at any age, they are uncommon before the age of 20 years and after 65 years.3
Modern treatments for first and second degree haemorr-hoids include sclerotherapy, rubber band ligation, and cryosurgery. However, each of these procedures is associated with certain complications. In sclerotherapy, the recurrence rate is approximately 15%, and complications may include hypochondriac pain due to entry of drug into the portal system, ulceration, and submucosal abscess formation. In Barron’s banding, if the band is applied too low into skin, it may lead to severe pain, discomfort, secondary haemorrhage, and ulceration. Cryosurgery is often followed by profuse, foul-smelling, watery discharge beginning within three hours of the procedure and lasting for 2 to 4 weeks, resulting in prolonged recovery.3 Thus, modern science has very lit-tle to offer in terms of the medical treatment of haemorrhoids.
Arshas is one of the Gudagata vikaras and can be correlated with haemorrhoids. Acharya Vagbhata states that Arshas are mamsankura (protrusion of mamsa) that obstructs the Guda marga and afflicts the person like an enemy.4 It is deerghakalanubandhi, dushchikitsa, tridoshaja, and occurs in a marma sthana, and therefore is considered one among the Ashta Mahagada.5
Arshas is manifested due to improper diet, sedentary lifestyle, prolonged standing, irregular sleep habits, and vegadharana, which disturbs the digestive system and cause constipation, leading to derangement of the trido-shas, mainly Vata dosha. The vitiated doshas localize in Gudavalli, Pradhana Dhamani and Mamsadhara Kala, thereby vitiating twak, mamsa, medas and rakta, resulting in Mahasrotodushti.6,7
Arsha formed within the Gudoushta (anus) is termed Abhyantara Arsha, which is associated with symptoms of Mamsankura in the Guda,Shula, Raktasrava.7,8,9 Acharya Sushruta has mentioned four treatment modalities for Arshas, namely Aushadha, Shastra, Kshara, and Agni Karma. Among these, Aushadha causes the least discomfort to the patient psychologically, physically and economically.10 Hence, effective management of this condition using Aushadha is the need of the hour.
Acharya Charaka, while outlining the uses of Saindavadya Taila,11 specifically mentions its application for Arshas (haemorrhoids). Therefore, in the present study, an attempt was made to evaluate the effect of Saindavadya Taila in the form of Guda Purana, with Kasisadi Taila taken as the control drug, as its efficacy in Arshas has already been established.11,12
Materials and Methods
This study was approved by the Institutional Ethics Committee under the reference number SJGAMC/ IEC/2022/SHALYA/03 on 10/10/2022. It was also registered with the CTRI under the reference number REF/2024/02/078782 and CTRI Registration No. CTRI/2024/08/072482.
Source of Data
Forty diagnosed patients with clinical features of Abhyantara Arshas (Internal haemorrhoids) who met the inclusion criteria and reporting to the Shalya Tantra OPD of S.J.G. Ayurvedic Medical College, Hospital and Research Centre, Koppal, were selected for the study.
Study Design
An open label, randomized controlled clinical trial. A total 40 cases of Abhyantara Arshas (Internal haemorrhoids) who met the eligibility criteria were randomly allotted into two groups: Group A and Group B with 20 patients in each group. A special case proforma was prepared, including history taking, physical examination, ano-rectal examination, and standard haemogram investigations.
Intervention
Group A was treated with Saindavadhya Taila Guda Pur-ana for seven days, while Group B received Kasisadi Taila Guda Purana for the same duration.
Inclusion Criteria
- Patients with Abhyantara Aarsha (Internal haemorrhoids).
- First and second degree internal haemorrhoids.
- Patients of either gender, aged 21 to 65 years, with a maximum of three internal haemorrhoids.
- Patients with Hb% > 8 g/dL.
Exclusion Criteria
- External and thrombosed pile mass.
- Third and fourth degree internal haemorrhoids.
- HIV and HBsAg positive patients.
- Patients diagnosed with conditions such as uncon-trolled diabetes, anal fissures, anal fistula, irritable bowel syndrome (IBS),ulcerative colitis, Crohn’s disease, tuberculosis, and rectal cancer.
Procedure (Taila Purana)
Poorva Karma: The procedure was explained to the patient in his/her own language, and informed consent was obtained. All required materials were prepared in advance. The patient was asked to lie comfortably in the left lateral position on the examination table, with the left leg extended straight, the right leg flexed at the knee and hip joints, and the head supported by the left hand, while the right hand rested on the right leg. The area was cleansed with sterile gauze dipped in warm water and then patted dry with a sterile dry gauze.
Pradhana Karma: Depending on the assigned group, 10 mL of lukewarm Saindavadhya Taila or Kasisadi Taila was loaded into a 10 mL syringe. A sterile red rubber catheter was fixed to the nozzle of the loaded syringe, and air bubbles were evacuated. The tip of the catheter and the anal canal were lubricated with the same Taila and gently inserted into the patient’s anal canal. The entire 10 mL of Taila was then slowly administered. The catheter was gently withdrawn, and a sterile gauze was placed at the site (Table1).
Details About Trial Drug (Table 1)
Paschat Karma: After administration of the Taila, the patient was asked to lie in a supine position. Both legs were then raised and slightly flexed at the knee joint a few times, followed by gentle tapping over the hips. After 10 minutes, the patient was advised to get up from the table.
Patients were instructed to take a Sitz bath with Triphala Kwatha for 15 minutes, twice daily, for seven days, in addition to following recommended Pathya-Apathya guidelines.
The same procedure was repeated daily for seven days.
Assessment Criteria
Assessment was carried out on the 1st day (before treatment), 7th day (after treatment), 14th day (Follow-up 1), and 21th day (Follow-up 2).
Parameters
a) Subjective Parameters
Bleeding13
Ø Grade 0 - No bleeding
Ø Grade 1 - Mild bleeding; occasional episodes (during defecation)
Ø Grade 2 - Moderate bleeding; frequent episodes (during defecation)
Ø Grade 3 - Severe bleeding; persistent bleeding even without defecation with fall in Hb level (<10 g/dL); requiring haematinics
Ø Grade 4 - Very severe bleeding; bleeding in the form of jets and splashes with severe fall in Hb level (<7 g/dL); requiring blood transfusion
Constipation14
Ø Grade 0 - No constipation (passing stool daily with normal consistency)
Ø Grade 1 - Mild constipation (passing stool daily but with hard consistency)
Ø Grade 2 - Moderate constipation (passing stool on alternate days with hard consistency)
Ø Grade 3 - Severe constipation (passing stool on 3rd day with hard consistency)
b) Objective Parameters
Size of the pile mass (pedicle size - proctoscopic evalu-ation)15
Ø Grade 0 - No pile pedicle visualized
Ø Grade 1 - Size smaller than a peanut
Ø Grade 2 - Size equivalent to a peanut
Ø Grade 3 - Size of a groundnut or larger
Number of the pile mass16
Ø Grade 0 - No pile mass
Ø Grade 1 - One pile mass
Ø Grade 2 - Two pile mass
Ø Grade 3 - Three pile mass
Statistical Tests
Repeated measures ANOVA was used for within-group comparisons, and the Mann-Whitney U test was applied for between-group comparisons. The data were then analyzed accordingly.
Results
This open-label, randomized controlled clinical trial included 40 patients, categorized into two groups: Group A and Group B, with 20 patients in each group. Group A was administered Saindavadhya Taila Guda Purana and Group B was administered Kasisadi Taila Guda Purana.
In this study, the maximum number of patients, 16 (40%), belonged to the 26-35 years age group. A total of 25 (62.5%) patients were male, 33 (82.5%) patients belonged to Hindu religion, 15 (37.5%) were housewives. Additionally, 32 (80%) patients were from the middle-class socioeconomic group, and 21 (52.5%) consumed mixed diet. Detailed demographic data are provided in Table 2.
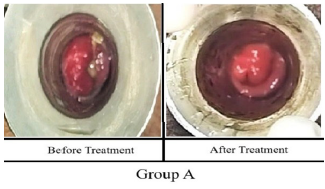
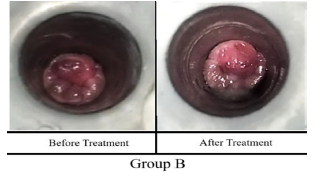
Clinical images before and after treatment for Group A and Group B are presented in Figure 1 and Figure 2, respectively.
Effect on Bleeding
Statistical analysis showed that comparisons within Group A and Group B, analyzed using repeated measures ANOVA, demonstrated a significant reduction in bleeding parameters (P=0.000; P <0.001).
Comparison between the groups using the Mann- Whitney U test revealed no statistically significant difference in bleeding at any time point. After treatment, both Group A and Group B had a mean score of 0.80 (SD = 0.523), with a U value of 200 and P=1.000 (P >0.05).
At follow-up 1, Group A recorded a mean score of 0.25 (SD = 0.444), while Group B showed a mean score of 0.20 (SD = 0.410), with mean ranks of 21 and 20, respectively (P=0.708; P >0.05).
At follow-up 2, the mean score was 0.20 (SD = 0.410) for Group A and 0.10 (SD = 0.308) for Group B, with mean ranks of 21.5 and 19.5, respectively (P=0.382; P >0.05).
These findings suggest that there was no statistically significant difference in bleeding levels between the two groups at any stage, indicating that both treatments provided comparable therapeutic effects.
Saindavadhya Taila helps in the reduction of bleeding, which can be attributed to the Raktastambhaka and Vrana Ropana properties of drugs like Saindhava Lavana, Bhallataka, and Tila Taila. The Lavana Rasa and Snigdha Guna of Saindhava Lavana, along with its Sheeta Virya and Madhura Vipaka, promote shoshana. Bhallataka, with its Katu Rasa, Tikshna Guna, and Ushna Virya, facilitates Sthambana and Shonitasthapana, while its Kashaya rasa aids Sandhanakara. Drugs like Shunti, Pippali, and Chitraka act as Sothahara, and their Ushna Virya and Katu Vipaka help in breaking down Shonita Sanghatam Binathi. The chemical constituents such as sodium chloride in Saindhava Lavana and gingerol in Shunti enhance circulation and promote tissue contraction, thereby helping prevent haemorrhagic episodes.
Kasisadi Taila also showed improvement in reducing bleeding, which can be attributed to its Prabhava. Kaseesa performs the functions of Vaatanulomana and Vranaropana.
Effect on Size of Mamsankura
Statistical analysis showed that comparisons within Group A and Group B, analyzed using repeated measures ANOVA, demonstrated a highly significant difference (P =0.000; P <0.001).
Comparison between the groups using the Mann- Whitney U test showed no statistically significant difference at after treatment, follow-up 1, and follow-up 2 (P >0.05), with P=0.096, P=0.127, and P=0.105, respectively.
After treatment, the mean rank for Group A was higher (23.00) compared to Group B (18.00).
At follow-up 1, the mean rank for Group A was 22.80 compared to Group B’s 18.20.
At follow-up 2, the mean rank for Group A was 22.83 compared to Group B’s 18.18.
These results suggest that there was no statistically significant difference in the reduction of mamsankura size between the two groups at any time point, although Group B showed a comparatively greater reduction by the second follow-up.
In Saindavadhya Taila, the slight reduction in the size of the pile mass may be due to the presence of drugs with Arshogna properties. Bhallataka, Chitraka, and Shunti possess Lekhana and Bhedana properties. These drugs, with their Katu Rasa, exhibit actions such shotahara, mamsa vilikhati, sleshma shamana, a Shunti possessi. Saindhava Lavana performs Kaphavishyandana, Shotahara, and Vranadoshahara. Chemical constituents such as Plumbagin in Chitraka and Bhilawanol in Bhallataka contribute to anti-inflammatory and tissue-reducing effects, aiding in the shrinkage of the piles.
In Kasisadi Taila, Danti and Kaseesa exhibit Arshogna properties. The Lekhana action of Citraka, Vidanga, and Karanja helps in reducing the size of the haemorrhoidal masses, through Lekhana Karma.
Effect on Number of Mamsankura
Comparison within Group A and Group B, analyzed with repeated measures ANOVA, showed no significant differences in the number of Mamsankura (P=0.167; P >0.05 for Group A and P=0.011; P >0.05 for Group B).
Comparison between the groups using the Mann- Whitney U test also showed no statistically significant differences (P >0.05).
After treatment:
Group A: mean = 2.1, SD = 0.718, mean rank = 20.95
Group B: mean = 2.05, SD = 0.605, mean rank = 20.05
U = 191 and P=0.784 (P> 0.05)
Follow-up 1:
Group A: mean = 2.05, SD = 0.686, mean rank = 20.90
Group B: mean = 2.0, SD = 0.649, mean rank = 20.10
U = 192, P=0.808 (P> 0.05)
Follow-up 2:
Both groups: mean = 2.0, SD = 0.649, mean rank = 20.50
U = 200, P=1.000 (P> 0.05)
These findings suggest that there was no statistically significant difference in the number of Mamsankura between the two groups at any point, indicating that both Group A and Group B experienced similar outcomes in relation to the number of Mamsankura.Both Saindhavadhya Taila and Kasisadi Taila may reduce the size of the haemorrhoidal mass and alleviate symptoms; however, complete elimination of multiple haemorrhoidal masses is challenging due to chronicity, vascular changes, recurrent irritation during defecation, Ama and Srotorodha. Additionally, a duration of only seven days of treatment may not be sufficient to produce a marked reduction in the number of Mamsankura.
Effect on Constipation
Comparison within Group A and Group B, analyzed using repeated measures ANOVA, showed a highly significant reduction (P=0.000; P<0.001).
Comparison between the groups using the Mann- Whitney U test showed no statistically significant differences at after treatment, follow-up 1, and follow-up 2, with P=0.343 (P> 0.05), P=0.157 (P> 0.05), and P=0.298 (P> 0.05), respectively.
After treatment: Group A mean rank = 22; Group B = 19
Follow-up 1: Group A mean rank = 22; Group B = 19
Follow-up 2: Group A mean rank = 21.5; Group B = 19.5
These findings indicate that although both groups showed a significant reduction in constipation scores, there was no significant difference between the groups at any time point, suggesting that both the treatment remedies were similarly effective in relieving constipation symptoms.
In Saindavadhya Taila, the use of Taila helps in Vatashamana and Vatanulomana. The Snigdhata of the Taila softens hard stools and facilitates their passage by lubricating the anal canal. Relief from constipation can also be attributed to the Deepana and Pachana properties of Shunti, Pippali, and Chitraka. The Katu Rasa, Ushna Virya, and Snigdha Guna of Shunti and Pippali help in Vibhandahara. Saidhava Lavana with Lavana Rasa, Aranala with Amla Rasa and Ushna Virya, and Tila Taila with its Snigdha and Vyavayi Guna helps in Vatanulomana. The presence of lactic acid in Aranala and gingerol in Shunti helps balance gut flora, reduce inflammation, and relieve constipation by promoting the natural expulsion of waste.
In Kasisadi Taila, the Lekhana and Virechana actions are due to Citraka and Snuhi Kşira. The Ushna Virya of Arka Kşira and Haratāla also contribute to Vatanulomana. Ingredients like Vidanga and Karanja, with their Katu Rasa and Kaphavātahara properties, support Deepana and Pachana actions.
The intragroup comparison results for Group A and Group B are given in Table 3.
Discussion
A review of Ayurvedic literature classifies Arsha as a Raktadushtijanya Vyadhi and includes it among the Ashta Mahagadas, indicating its difficult nature to cure. The seriousness of Arsha is underscored by its potential complications. Sushruta noted that untreated Arsha could result in significant blood loss, Samgrahani, Kasa, Shwasa and even severe outcomes such as loss of vision.
Sushruta further states that Arsha should be treated according to the principles of Bhaishaja, Kshara Karma, Agni Karma, and Shastra Karma, based on the severity of symptoms. In modern terms, Arsha corresponds closely to the clinical condition known as haemorrhoids. Among the four modes of treatments mentioned, Aushada causes least discomfort to the patient psychologically, physically, and economically. Hence effective management of this condition using an Aushadha is the need of the hour.
Acharya Charaka, while outlining the uses of 'Sainda-vadya Taila' specifically mentions its application in the management of Arshas. Therefore, in the present study, an attempt was made to evaluate the effect of Saindavadya Taila administered in the form of Guda Purana, with Kasisadi Taila taken as control, as its efficacy in Arshas has already been established.
Probable Mode of Action of Saindavadhya Taila Purana on Arshas
1. Vatanulomana
2. Agni Deepana
3. Arsho Ankura Samkocha
1. Vatanulomana: Basti is considered the primary treatment for Vata imbalance, with Taila being the preferred medication. Administering Taila through the anal route directly targets the Pakwashaya, the principal site of Vata. This helps to balance aggravated Vata, and relieve symptoms. Drugs like Saindhava Lavana, which is Vata Pradhana Tridoshagna, Shunti with Ushna Guna, and Pippali also act as Vatanulomana, helping in relieving symptoms such as constipation, which is the main etiological factor for Arshas.
2. Agni Deepana: Taila Purana is performed in the left lateral position as recommended in Ayurvedic texts. According to Acharya Gangadhara, Agni, Grahani, and Nabhi are situated towards the left side. Jejjata also comments that Agni is located on the left side near the Nabhi, and Guda has a left-sided relation with the Sthoolantra. Hence, Basti Dravya can reach the large intestine and Grahani, as they are present in the same level. Thus, it can be inferred that Saindavadhya Taila may act on Agni and support its proper functioning. The Saindavadhya Taila used in the treatment possess Deepana and Pachana properties. Most of its ingredients such as Shunti, Pippali, Chitraka, and Bhallataka have Ushnna Veerya and Katu Rasa. All these contribute significantly to the Deepana and Pachana. This helps in normalizing digestion and softening stools, thereby reducing pressure on the rectal plexus. This effect is crucial for alleviating discomfort associated with internal haemorrhoids.
3. Arsho Ankura Samkocha: Acharya Charaka ment-ions that in the left lateral position, relaxation of the Gudavalees and alignment of Grahani and Guda allow the Basti fluid to reach the target organs. Matra Basti mainly purifies the Pureeshadharakala, thereby promoting healing in the rectal region. The Lekhana effect of Saindavadhya Taila helps reduce haemorrhoidal mass. Chitraka primarily performs Lekhana, which helps in reducing Shopha, while Bhallataka possesses Bhedana, Vrana hara, and Arshogna properties. Together, these actions assist in shrinking the haemorrhoidal mass by eliminating accumulated waste.
Mode of Action Based on Analytical Study of Sainda-vadhya Taila
1. Local Absorption: The specific gravity (0.908 g/cm³) and moderate viscosity (23.8 mPa.s) of Saindavadhya Taila facilitate efficient absorption through the rectal mucosa, thereby enhancing the bioavailability of its active ingredients.
2. Anti-inflammatory and Analgesic Effects: The presence of free fatty acids (acid value: 3.72 mg) contributes to significant anti-inflammatory and analgesic actions, which help to reduce swelling, pain, and irritation in the haemorrhoidal region.
3. Venotonic Properties: Unsaturated fatty acids (iod-ine value: 55.374 mg) strengthen haemorrhoidal veins, reducing congestion and size of haemorrhoidal masses.
4. Lubrication and Stool Softening: The oil’s visco-sity provides adequate lubrication, thereby minimizing friction and trauma during bowel movements, thus aiding in prevention of bleeding.
5. Enhanced Healing: Antioxidant properties (low peroxide value: 10.937 meq/kg) promote tissue rep-air and prevent further inflammation, thus strength-ening rectal tissues.
6. Detoxification: The saponification value (59.0 mg) indicates a cleansing effect, removing impurities from the rectal area and supporting healing.
7. Systemic Effects: Absorption through the haemorrhoidal veins can enhance digestive function and reduce systemic inflammation, thereby addressing underlying causative factors of haemorrhoids.
8. Comprehensive Healing: Saindavadhya Taila offers a holistic approach by reducing inflammation, improving circulation, lubricating the anal canal, enhancing healing, and providing systemic benefits.
Mode of Action According to Contemporary Science
The absorption of Taila is enhanced with longer reten-tion times of Basti dravya. Modern science indicates that the rectum has a rich supply of blood and lymph, and drugs can readily penetrate the rectal mucosa, similar to other lipid membranes. In the context of Basti (enema), lipid-soluble and unionized substances are efficiently absorbed through the trans-rectal route. The concentration gradient of Matra Basti dravya is higher in the intestinal lumen than in the rectal venous plexus, facilitating absorption. This plexus is divided into the internal and external venous plexuses. The internal venous plexus, located in the submucosal layer of the anal canal, drains into the superior rectal vein, which communicates with the external venous plexus. Basti dravya is absorbed from the external plexus in three parts: the lower section drains via the inferior rectal veins into the internal pudendal vein; the middle section drains via the middle rectal vein (which has tributaries draining the bladder, prostate, and seminal vesicle) into the internal iliac vein; and the upper section drains via the superior rectal vein into the inferior mesenteric vein, a tributary of the portal vein. The portion absorbed from the lower rectum directly enters systemic circulation through the middle and inferior haemorrhoidal veins. This indicates efficient absorption due to the increased vascularity in this region. The drugs absorbed through the haemorrhoidal veins alleviate obstructions, thereby reducing the haemorrhoidal mass.
Probable Mode of Action of Triphala Kwatha Sitz Bath
Triphala Churna is Tridoshashamaka and possesses anti-inflammatory, analgesic, and antibacterial properties. Triphala Kwatha sitz bath helps relieve pain by relaxing the anal sphincter. The warm temperature of Kwatha aids in improving blood circulation. It also helps main-tain hygiene, and provides relief from burning sensation. Kegel exercises were advised during sitz bath to enhance the strength of the sphincter muscles.
Pathya
A soft and fiber-rich diet was advised for all patients. Die-tary fiber consists of soluble and insoluble components. Insoluble fiber provides bulk to the stool, and soluble fiber provides a gelatinous quality. Certain fibers also nourish beneficial gut bacteria, which in turn produce short-chain fatty acids. These short-chain fatty acids feed the cells in the colon, thereby improving digestion and relieving constipation. Thus, a fiber-rich diet aids in proper digestion and helps prevent constipation and hard stools.
Conclusion
The present comparative clinical study included 40 patients diagnosed with Abhyanatara Arsha, randomly assigned to two groups. Group A was treated with Saidavadhya Taila and Group B with Kasisadi Taila for seven days.
Käsisadi Taila is a result-oriented local treatment for Arsha, as mentioned by Acharya Sušruta in Arśa Roga Cikitsa. Analytical findings suggest that Käsisadi Taila is more acidic than Saindavadhya Taila. Additionally, most of the ingredients in Käsisadi Taila possess Uşņa, Tiksna, Lekhan, and Shothahara properties. On intra-group comparison, both Group A and Group B showed significant improvement in bleeding and constipation. Group B showed significance improvement in the size of Mamsankura, whereas both groups were not significant in reducing the number of Mamsankura.
On inter-group comparison, there was no statistically significant difference between Group A and Group B in bleeding, size, and number of Mamsankura, and relief in constipation. However, based on sum of ranks, Group B showed greater improvement in bleeding, reduction in size of Mamsankura, and relief in constipation. Overall, 70% of patients in Group A showed moderate to marked improvement, while 80% of patients in Group B experienced similar improvement. Both groups demonstrated positive outcomes, but Group B had a slightly higher overall response rate.
Therefore, based on observation and study results, it can be concluded that Kasisadi Taila demonstrated comparatively better effectiveness in most clinical parameters than Saidavadhya Taila, except in reducing the number of Mamsankura.
Funding
Nil
Conflicts of interest
None
Acknowledgment
1. Dr. Anisha S Ashraf, Assistant Professor, Depart-ment of Shalya Tantra, Shree Jagadguru Gavisiddes-hwara Ayurvedic Medical College and Hospital, Koppal - For Scientific support.
2. Dr. Anusha K, Final year PG Scholar, Department of Shalya Tantra, Shree Jagadguru Gavisiddes-hwara Ayurvedic Medical College and Hospital, Koppal- For Technical support.
Supporting File
References
1) Das S. A concise textbook of surgery. 6th edition. Chapter 46. Kolkata: S Das, Kolkata; 2010. p. 959.
2) Lohsiriwat V. Hemorrhoids: From basic pathophy-siology to clinical management. World J Gastroen-terol 2012;18(17):2009-17.
3) Bhat MS. SRB’S Manual of Surgery. 5th edition. New Delhi: Jaypee Brothers Medical Publishers; 2016. p. 971
4) Bhat MS, SRB’S Manual of Surgery. 5th edition. New Delhi: Jaypee Brothers Medical Publishers; 2016. p. 972-974.
5) Pandit Hari Sadasiva Sastri Paradikara Bhisagacharya, editor. Sarvanga Sundara, Commentary. Nidan-asthana 7/1, Arunadatta, Astanga Hrudaya Reprint ed. Varanasi: Choukambha Surabharati Prakashan; 2016. p. 490.
6) Acharya YT, editor. Nibandha Sangraha, Commentary. Sutrasthana 33/4, Sri Dalhanacharya, Sushruta Samhita Reprint ed. Varanasi: Chaukhambha Samskrutha Samsthana; 2014. p. 144.
7) Acharya YT, editor. Nibandha Sangraha, Commen-tary. Nidhanasthana 2/4, Sri Dalhanacharya, Sushruta Samhita Reprint ed. Varanasi: Chaukhambha Samskrutha Samsthana; 2014. p. 270.
8) Kumar HP. Recent advances in the management of Arshas/haemorrhoids. 1st Edition. Hassan: Sai Cha-ran Publications; 2004. p. 14.
9) Acharya YT, editor. Nibandha Sangraha, Commen-tary. Nidhanasthana 2/10, Sri Dalhanacharya, Sushruta Samhita Reprint ed. Varanasi: Chaukham-bha Samskrutha Samsthana; 2014. p. 270.
10) Acharya YT, editor. Nibandha Sangraha, Commen-tary. Nidhanasthana 2/11, Sri Dalhanacharya, Sushruta Samhita Reprint ed. Varanasi: Chaukha-mbha Samskrutha Samsthana; 2014. p. 270.
11) Acharya YT, editor. Nibandha Sangraha, Commen-tary. Nidhanasthana 6/3, Sri Dalhanacharya, Sushruta Samhita Reprint ed. Varanasi: Chaukham-bha Samskrutha Samsthana; 2014. p. 430.
12) Acharya YT, editor. Ayurved Dipika, Commentary. Chikitsasthana 27/45-46, Agnivesa, Charaka Sam-hita, with Chakrapaanidatta. Reprint ed. New Delhi: Chaukhambha Surbharati Parkashan; 2016. p. 615.
13) Acharya YT, editor. Nibandha Sangraha, Commen-tary. Chikitsasthana 6/12, Sri Dalhanacharya, Sushruta Samhita Reprint ed. Varanasi: Chaukham-bha Samskrutha Samsthana; 2014. p. 432.
14) Khan MA, Khan ZA, Parray, FQ, et al. PNR-Bleed classification and the prospects of future research for the management of hemorrhoids. Indian J Colo- Rectal Surg 2021;4(3):68.
15) Bidwai V. Kasisadi Tail Basti in Arsha. Interna-tional Journal of Science and Research 2021;10(5): 1281-84.
16) Poonam A, Shriniwas G, Rajender S, et al. Manage-ment of Abhyantara Guda-Arsha (Grade-2) with ‘Kasisadi Taila - Matrabasti’ and Triphla Gugglu - A case study. International Ayurvedic Medical Journal 2022;4:1088-1093. Available from: http:// www.iamj.in/posts/images/upload/1088_1093.pdf